Health spending rose faster than GDP in almost all European countries over the past decade. This box investigated most notable long-term drivers of real spending on health care: demographic effects, income effects and other cost pressures.
This box is based on OECD health spending and GDP data from June 2013 .
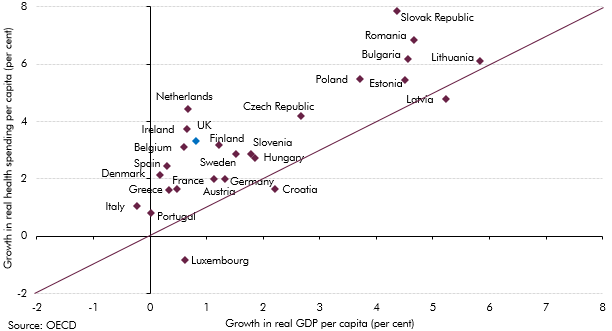
Health spending has risen faster than GDP in almost all European countries over the past decade (almost all dots are above the diagonal line in Chart C). Our central long-term projections show that trend continuing in the UK, with health spending expected to be the largest source of age-related pressure on the public finances. The sensitivity analysis we present shows that assumptions about what drives changes in health spending as a share of GDP – which we capture by varying our assumption about relative productivity growth in the health sector – are incredibly important. In Annex B of our 2012 FSR, we reviewed a number of sensitivities around our central health spending projection. This box provides an update on that analysis, drawing on a number of reports published over the past three years.
Chart C: Growth of real health spending and GDP per capita (2000 to 2012)
The academic literature identifies three main long-term drivers of real spending on health care:
- demographic factors: the effect of the changing age structure of the population, survivor status and death-related costs. We capture these effects in our central projections. Implicitly, we assume that healthy life expectancy rises proportionately with total life expectancy. An alternative assumption would be to assume that more of the additional years of life are spent in better health;
- income effects: the fact that health care is a ‘normal good’, meaning people demand more as incomes rise. This drives real spending, but only affects spending as a share of GDP if the income elasticity is greater or less than one. Our central projections are consistent with an income elasticity of one; and
- other residual factors: non-demographic factors such as technological advances, relative price/productivity effects and policy or lifestyle changes. Our sensitivity analysis for the effects of lower health sector productivity captures a key residual factor that may push up health spending in future.
Studies of past trends in health spending show that the income effect is the biggest driver of real terms increases – though with an estimated elasticity typically close to one, this does not account for the rising share of GDP devoted to health spending. Demographic effects have explained little of the past change, although they are expected to account for much more in the future as populations age. As such, it has been residual factors that have largely explained the past rise in health spending as a share of GDP.a
In 2013, the OECD published long-term health spending projections that incorporated estimates of residual excess cost growth explicitly. It presented two scenarios: a ‘cost pressure’ scenario, in which excess cost growth was set at 1.7 per cent a year (based on an econometric estimate of the impact of technology, relative prices and other factors on health care spending) and a ‘cost containment’ scenario, in which that growth rate was assumed to drop to zero over time (on the assumption that policymakers will be able to address these pressures).b Our lower health productivity scenario assumes excess cost growth of 1.1 per cent a year, so the higher residual projected by the OECD suggests other factors have also been at play.
Technological advancements are potentially one such additional driver of excess cost growth. Unlike most industries, technological innovations are generally cost-escalating rather than cost-containing. For example, the Commission’s 2015 Ageing Report quotes estimates that attribute from around a quarter to around three quarters of health expenditure growth in the industrialised countries to technological change. Such advancements can also increase patient demand, without, in most cases, reducing labour input. For example, new technologies will increase costs if they treat conditions for which there was previously no, or no effective, treatment. Even if an advance lowers the unit cost of treatment, spending can increase if that treatment becomes more widely used, addressing previously unmet demand. Morbidity associated with chronic conditions is also likely to pose an increasing fiscal burden, both due to ageing but also to changing lifestyles. Given the importance of trends in health spending for fiscal sustainability, these are issues we will return to in greater depth again in the future.
There is no consensus over the contribution of demographic, income and residual factors among the drivers of health care spending over the long term (Chart D), but estimates that include a residual component for the effects of low productivity or the impact of technology developments tend be larger than those that focus only on demographic and income-related factors.
Chart D: Long-term projections of changes in health care spending (2020 to 2060)